The Role of Telehealth in Modern Medicine
Introduction to Telehealth
Telehealth represents a broad range of technologies and services that enhance patient care, encompassing everything from video consultations to mobile health applications. While often used interchangeably with telemedicine, telehealth is a more inclusive term that encompasses the entire spectrum of remote healthcare delivery, including education, training, monitoring, and support for both patients and providers.
The significance of telehealth has surged in recent years, particularly in response to the growing demand for accessible healthcare solutions. Innovative communication technologies, such as high-definition video conferencing, secure messaging platforms, and mobile health applications, have transformed how patients interact with healthcare professionals. These advancements allow individuals to receive timely care regardless of geographical barriers, ultimately contributing to improved health outcomes and reduced service costs.
Telehealth’s evolution has been accelerated by the proliferation of smartphones and other digital devices, empowering patients to take a more active role in managing their health. This empowerment leads to better engagement, adherence to treatment plans, and proactive health measures. The use of telehealth services is not limited to routine consultations; it also extends to chronic disease management, mental health services, and post-operative follow-ups, demonstrating its versatility and comprehensive nature.
As healthcare systems continue to grapple with challenges such as provider shortages and the need for more efficient service delivery, telehealth emerges as a crucial solution. With the support of technology, healthcare providers can extend their reach, offering specialized care to underserved populations. The increasing importance of telehealth in modern medicine is evident, paving the way for a new paradigm in healthcare delivery that prioritizes accessibility and convenience for patients across diverse backgrounds.
Benefits of Telehealth
Telehealth has emerged as a significant component of modern medicine, offering numerous benefits that enhance healthcare delivery for patients and providers alike. One of the foremost advantages is increased access to healthcare, particularly for individuals residing in remote or underserved areas. By utilizing telehealth services, patients can consult with healthcare professionals without the burden of traveling long distances, effectively bridging gaps in care and ensuring that specialized services are accessible to all, regardless of their geographic location.
Convenience is another key benefit associated with telehealth. It allows flexible scheduling of appointments and can often accommodate patients’ busy lifestyles. Both patients and healthcare providers can engage in consultations from their respective locations, eliminating time lost in waiting rooms and reducing the overall time commitment associated with in-person visits. This ease of access not only improves patient satisfaction but also enhances provider workflow and efficiency.
From an economic perspective, telehealth presents potential cost savings for both patients and healthcare systems. Patients save on travel expenses and time off work, while healthcare providers can streamline operations, leading to reduced overhead costs. A report by the American Hospital Association indicates that telehealth can decrease the need for in-person visits, which not only saves money but also optimizes resource allocation within healthcare facilities.
Improved patient engagement is another hallmark of telehealth. Utilizing digital platforms, healthcare providers can maintain regular communication with patients, encouraging adherence to treatment plans and follow-up appointments. Studies have shown that patients who engage through telehealth are more likely to participate in their health management, leading to better health outcomes. Overall, the integration of telehealth into healthcare systems has demonstrated a transformative potential, positively impacting the accessibility, efficiency, and effectiveness of care delivery.
Challenges and Limitations of Telehealth
While telehealth has emerged as a transformative force in modern medicine, its adoption is not without challenges and limitations that must be addressed to maximize its potential benefits. One of the foremost obstacles is the disparity in access to technology. Not all patients possess the necessary devices or internet connectivity to utilize telehealth services effectively. This digital divide can disproportionately affect rural and underserved populations, exacerbating existing healthcare inequalities.
In addition to access issues, privacy concerns pose significant challenges for telehealth. Patients may feel apprehensive about sharing sensitive medical information over digital platforms, fearing that their data may be compromised or misused. This skepticism can hinder patient engagement, leading to reluctance in utilizing telehealth, particularly amongst older generations who may not be as technologically savvy.
Regulatory issues further complicate the landscape of telehealth. Variations in state laws regarding telemedicine practices can create confusion for healthcare providers. For instance, some states may require in-person visits before establishing a telehealth relationship, while others impose restrictions on prescribing medications through virtual consultations. These regulatory hurdles can limit the scope of care that telehealth can provide, ultimately affecting patient outcomes.
Finally, the need for a personal touch in patient care cannot be understated. Many patients and providers value face-to-face interactions, which offer nonverbal cues and emotional support that technology may not fully replicate. For example, patients recovering from serious illnesses often benefit from the comfort of being physically present with their healthcare provider, a nuance that virtual consultations can struggle to convey. Balancing technological innovation with the inherent need for human connection remains a core challenge in the telehealth arena.
Telehealth During the COVID-19 Pandemic
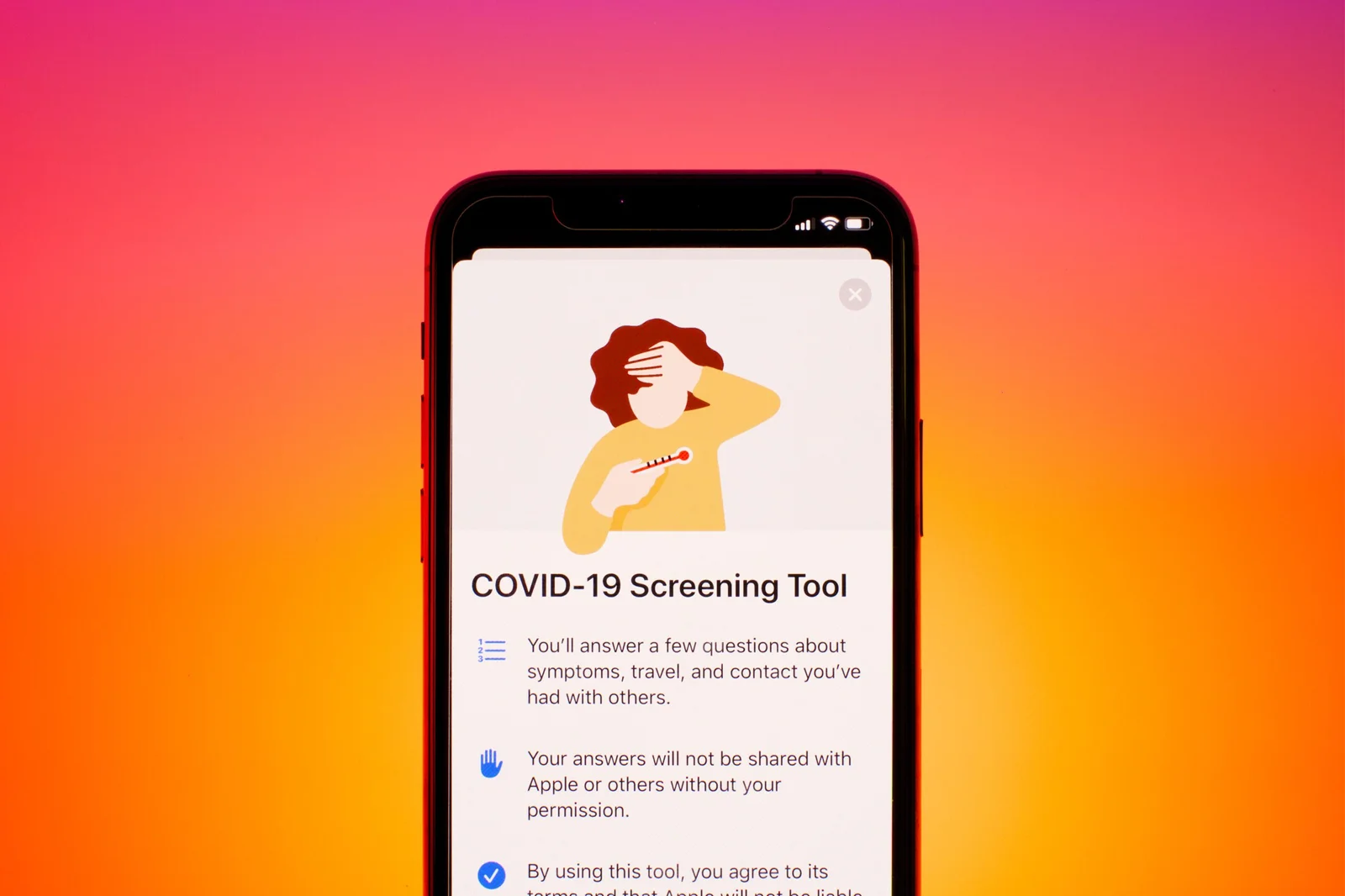
The COVID-19 pandemic has profoundly transformed the landscape of healthcare, catalyzing a significant surge in the utilization of telehealth services. As lockdown measures were implemented and social distancing became commonplace, healthcare delivery faced unprecedented challenges. In response, telehealth emerged as a vital tool to mitigate the overload on healthcare systems, allowing for remote consultations and continuity of care. This shift not only addressed immediate patient safety concerns but also ensured that those with chronic illnesses could continue receiving necessary medical attention without interruption.
During the early stages of the pandemic, a rapid expansion of telehealth services was facilitated by emergency measures instituted by health authorities and regulatory bodies. For instance, the U.S. Department of Health and Human Services waived certain HIPAA requirements, allowing providers to use a broader range of communication technologies, including non-secure platforms. This flexibility enabled a swift transition from in-person visits to virtual consultations, providing patients with timely medical guidance while minimizing the risk of virus transmission.
The increase in telehealth consultations spanned various specialties, ranging from primary care to mental health services. Providers quickly adapted to the new mode of engagement, utilizing video calls, phone consultations, and secure messaging to connect with patients. This adaptation not only allowed for ongoing evaluations of patient conditions but also represented a critical development in maintaining psychological support during a period of heightened anxiety and isolation.
Moreover, the pandemic underscored the importance of incorporating telehealth into mainstream healthcare practices. As both patients and providers recognized its benefits—such as convenience, accessibility, and efficiency—it sparked discussions regarding its permanence post-pandemic. Regulatory changes potentially indicate a future where telehealth continues to play an essential role in healthcare delivery, expanding access to services and improving overall patient outcomes. Thus, the COVID-19 crisis served as both a catalyst for change and a pivotal moment in the evolution of telehealth.
Future Trends in Telehealth
As the landscape of healthcare continues to evolve, telehealth is poised to integrate several transformative trends that reflect advancements in technology and patient care. One of the most significant trends is the incorporation of artificial intelligence (AI) into telehealth services. AI can enhance diagnostic accuracy, improve patient triage processes, and provide personalized health recommendations based on individual patient data. By leveraging AI algorithms, healthcare providers can offer more tailored services, making the virtual healthcare experience more efficient and effective.
Remote monitoring technologies are also set to become a cornerstone of telehealth, allowing healthcare providers to track patients’ vital signs and health metrics in real-time. Wearable devices that monitor heart rates, blood pressure, and other critical health indicators can transmit data directly to healthcare professionals. This continuous flow of information enables timely interventions and reduces the need for in-person consultations, particularly for chronic disease management. As these technologies become increasingly sophisticated, they will contribute to a more proactive approach to healthcare delivery.
Furthermore, the potential for personalized medicine through telehealth channels is gaining traction. With advancements in genomics and data analytics, healthcare providers can use telehealth platforms to provide customized treatment plans that cater to the unique genetic makeup of each patient. This shift towards personalization not only improves treatment outcomes but also enhances patient engagement and satisfaction, as individuals receive care tailored specifically to their health needs.
Post-pandemic, the role of telehealth is unlikely to diminish; rather, it is expected to evolve significantly. As public acceptance of telehealth increases, legislative support and reimbursement policies will likely adapt to facilitate its growth. In this regard, telehealth may not only persist but thrive as an integral part of modern medicine, reshaping how healthcare services are delivered and accessed across the globe.
Telehealth Regulations and Policies
The landscape of telehealth regulations and policies is complex and varies significantly across different regions. As telehealth continues to gain traction, understanding these regulations becomes essential for both healthcare providers and patients. One of the most critical components of telehealth policy is reimbursement. In many areas, insurance companies are adjusting their reimbursement policies to include telehealth services, which is crucial for ensuring that providers are compensated for remote care. However, discrepancies in coverage exist, as some insurers may not reimburse for services delivered via telehealth or may impose limitations on the types of conditions that qualify for remote consultations.
Licensing requirements further complicate telehealth practices. Healthcare providers who wish to offer telehealth services must often adhere to the regulations of the states or countries where their patients reside. This can mean that a provider licensed in one state may not legally treat a patient in another, unless they obtain additional licenses. Some regions have made strides towards more streamlined regulations, yet the current state of licensure remains a significant barrier for many providers looking to expand their practices.
The impact of recent legislative changes cannot be overlooked, as policymakers have begun to recognize the efficiency and necessity of telehealth services, particularly during the COVID-19 pandemic. Temporary measures were implemented to facilitate easier access to telehealth, and there is an ongoing discussion regarding the permanence of these changes. Issues such as privacy, security, and access equity continue to shape the future development of telehealth policies. As more stakeholders engage in these discussions, the evolution of telehealth regulations will play a key role in defining how healthcare is delivered in the modern era.
Patient Perspectives on Telehealth
Telehealth has emerged as a transformative component of modern medicine, providing patients with greater access to healthcare services. In recent years, numerous surveys have sought to gauge patient experiences with telehealth, revealing a range of opinions and satisfaction levels. Many patients appreciate the convenience telehealth affords them, allowing for appointments from the comfort of their homes. This accessibility is particularly beneficial for those with mobility issues or those residing in rural areas where healthcare facilities may be distant.
Satisfaction levels among telehealth users are generally high. According to recent studies, a significant majority of patients reported being satisfied with their telehealth consultations. They valued reduced travel time and the ability to consult with specialists who might be geographically unreachable. Additionally, telehealth platforms often incorporate messaging features, allowing patients to communicate with providers more easily, which can enhance overall care continuity. Providers also benefit, as such interactions can lead to more timely interventions and follow-ups.
However, while many patients have embraced telehealth, concerns remain. Some individuals report feelings of disconnection during virtual consultations, citing the absence of in-person interaction as a potential barrier to building trust with healthcare providers. Others worry about technological issues that may interfere with their appointments, such as a lack of familiarity with the software or poor internet connectivity. Privacy concerns also loom large, as patients question the security of their personal health information transmitted through these platforms.
Ultimately, patients’ perspectives on telehealth showcase a blend of appreciation for its benefits and caution regarding its limitations. As telehealth continues to evolve, ongoing dialogues between providers and patients will be essential to address these concerns and enhance the overall healthcare experience, ensuring that telehealth services meet the needs of all patients effectively.
Provider Perspectives on Telehealth
As telehealth continues to infiltrate modern medicine, healthcare providers have had to adapt their practices significantly. The rise of virtual consultations presents numerous workflow changes, compelling providers to pivot from traditional face-to-face interaction to a model that incorporates digital platforms. This shift entails not only mastering new technologies but also re-evaluating the approach to patient care and engagement.
Training needs have emerged as a crucial factor in the successful integration of telehealth. Providers often require additional education to effectively utilize telehealth platforms and tools, which can sometimes lead to apprehension. Moreover, as healthcare evolves, ongoing training ensures that practitioners remain proficient in delivering quality care to their patients through virtual mediums. Providers must learn how to conduct thorough assessments and maintain effective communication in a virtual environment, which differs from the nuances of in-person consultations.
Despite these challenges, many healthcare professionals recognize the benefits telehealth brings to their practice. Increased accessibility to healthcare services allows for timely interventions, particularly in underserved populations. Additionally, telehealth can improve patient adherence to follow-up appointments, as it often reduces the barriers associated with transportation and scheduling. For some providers, the flexibility and efficiency of telehealth provide a valuable means to manage their workload better.
However, concerns regarding patient rapport and quality of care remain prevalent among medical professionals. Establishing trust and a connection with patients can be challenging via telecommunication, sometimes resulting in missed non-verbal cues that are easily observed in person. Consequently, providers may worry about the potential impact on diagnosis and treatment efficacy.
In conclusion, while telehealth presents unique opportunities and challenges for healthcare providers, its successful integration necessitates adaptability, training, and a strong commitment to maintaining high-quality patient care.
Conclusion: The Future of Telehealth in Medicine
The integration of telehealth into modern medical practices has markedly transformed patient care and accessibility. As highlighted in the previous sections, telehealth offers significant advantages including convenience, increased access to specialists, and enhanced efficiency in managing chronic conditions. Nevertheless, the evolution of telehealth presents challenges that must be navigated for its long-term success. Ensuring equitable access to technology, addressing privacy concerns, and providing adequate training for healthcare providers are imperative steps to bolster telehealth services.
Looking ahead, the future of telehealth in medicine is vibrant yet requires ongoing development. One critical aspect lies in striking a balance between conventional healthcare practices and telehealth solutions. In-person visits are essential in certain scenarios, particularly for diagnostic evaluations or when physical examinations are necessary. Therefore, a hybrid approach—incorporating both traditional and telehealth modalities—could provide the most comprehensive care for patients, catering to individual needs while utilizing the benefits of technology.
Furthermore, fostering ongoing dialogue among healthcare professionals, policymakers, and patients is vital to enhance telehealth services. As innovations continue to emerge, stakeholders must collaboratively assess how telehealth can be optimized in various healthcare settings. This includes investigating alternative reimbursement models, integrating telehealth into existing healthcare frameworks, and ensuring regulatory compliance that aligns with evolving technological landscapes. Overall, the progression of telehealth represents a pivotal shift in modern medicine, offering an opportunity to enhance patient-centered care and improve health outcomes across diverse populations.
In summary, the path forward for telehealth is filled with potential. By addressing existing challenges, fostering collaborative efforts, and effectively combining traditional practices with telehealth innovations, the medical field can significantly advance its service delivery, ultimately leading to improved patient experiences and health results.
